Key Takeaways
- GLP-1 agonists like Semaglutide, Tirzepatide, and Retatrutide not only assist in blood sugar control but also significantly contribute to weight management and offer broader health benefits.
- Side effects of GLP-1 agonists commonly include gastrointestinal discomfort, but careful management and consideration of contraindications are essential for safe and effective treatment.
- Advancements in drug delivery systems, such as oral GLP-1 agonists and once-weekly injections, aim to improve patient adherence and convenience, enhancing the overall management of chronic conditions like diabetes and obesity.
If you’re seeking effective diabetes or obesity treatment, understanding GLP-1 agonists is key. Drugs like Semaglutide and Tirzepatide offer promising benefits for blood sugar control and weight loss. This article dives into how they work, what to expect, and why they might be a suitable option for you, helping you cut through the noise and focus on your health goals.
Exploring the Spectrum of GLP-1 Agonists
The introduction of GLP-1 agonists has revolutionized the treatment and management of diabetes as well as obesity. Medications such as Semaglutide, Tirzepatide, and Retatrutide offer distinct advantages in managing these conditions. They are particularly effective not only in controlling blood sugar levels, but also play a significant role in weight reduction and enhancing overall health.
Our analysis will delve into the characteristics of some key drugs within this category to understand their unique roles in addressing issues related to diabetes and obesity.
Semaglutide: A Versatile Player
Sema glutide has emerged as a dynamic contributor among GLP-1 agonists, receiving FDA approval for its role in managing type 2 diabetes, combating chronic kidney disease and aiding weight loss. The introduction of oral semaglutide tablets represents an important advancement in the ease of diabetes care. Semaglutide’s endorsement by the FDA for weight management testifies to its considerable effectiveness in helping individuals reach their desired weights.
The advent of oral semaglutide provides multiple advantages.
- It integrates effortlessly into patients’ day-to-day regimen, facilitating smoother control over complex health conditions.
- Its user-friendly nature combined with proven results have made it widely accepted among both medical professionals and those they treat.
- It contributes valuable benefits in addressing chronic kidney injury prevention and treatment plans.
A key factor behind Semaglutide’s proficiency at improving blood sugar levels is that it functions alongside long acting insulin to maintain consistent blood sugar regulation throughout the day. This harmonious relationship enhances Semagultides position as an essential component within current strategies aimed at treating diabetes effectively without sacrificing convenience.
In demonstrating flexibility, this medication can adapt to meet various treatment requirements — serving either as a solitary therapeutic option or accompanying other medications prescribed for managing diabetes symptoms. With ongoing progressions emerging from pharmaceutical researches development efforts, the application range of Semagliptide will likely continue expanding solidifying itself Informed our array of tools available tackling obesity complications related diabetic conditions.
Tirzepatide: The Dual Action Agent

In the quest for superior blood sugar control, Tirzepatide emerges as a striking dual action agent. Its innovative approach targets not one, but two crucial receptors: the glucose-dependent insulinotropic polypeptide (GIP) and the glucagon-like peptide-1 (GLP-1). The FDA’s approval in May 2022 for the treatment of type 2 diabetes marked a milestone in diabetes therapeutics, highlighting Tirzepatide’s potential to reshape diabetes management strategies.
The dual mechanism of action of Tirzepatide provides an edge in achieving glycemic targets, with studies indicating superior glycemic control and noteworthy weight reduction benefits for patients. This dual glucose-dependent insulinotropic capability means that Tirzepatide can more comprehensively address the complex interplay of hormones that regulate blood sugar levels.
For patients who have not achieved their treatment objectives with other diabetes medications, Tirzepatide as a combination therapy presents a hopeful substitute. Its ability to reduce food intake by enhancing satiety further supports individuals in their weight management efforts, a common challenge among those with type 2 diabetes.
The influence of Tirzepatide goes beyond the clinical sphere, providing hope for a future with more effective diabetes management and reduced complications. By harnessing the power of dual receptor activation, Tirzepatide stands as a testament to the innovative strides being made in diabetes care.
Retatrutide: Emerging Contender

Retatrutide, an innovative tri-agonist compound, is showing promising potential in the arena of health care. With its distinctive strategy for targeting receptors—namely those receptive to GIP, GLP-1, and glucagon—it stands out as a progressive option for the treatment of diabetes and obesity-related issues. A phase 2 study on obesity lasting 48 weeks revealed that Retatrutide could elicit up to a 24.2% reduction in weight, indicating significant capabilities in the realm of weight control.
By stimulating three different hormonal pathways simultaneously with Retatrutrude’s intervention comes effective blood sugar regulation alongside appetite suppression efforts which collectively lead to notable weight loss accomplishments. Advantages stemming from this medication include:
- Managed levels of glucose
- Dampened hunger signals
- Extended periods of fullness post meals
- Organic decrease in caloric consumption
Positive influences concerning cases concerned with excess body mass.
While it has garnered attention primarily within spheres addressing overweight issues, Retratruride’s merits regarding diabetes management should not be overlooked. It holds promise due to its facilitation of insulin secretion combined with glycemic control—a prospect potentially transforming diabetes care through an encompassing methodology towards condition maintenance.
Inquiries persist about how safe Retaratrutride’s multi-receptor approach may be considering specific concerns such as medullary thyroid cancer or kidney function results, particularly given that novel therapies always necessitate thorough scrutiny along ongoing research determination before cementing their roles within therapeutic disciplines.[full_image]
Exenatide: The First Market Entrant

Exenatide, a pioneer among the GLP-1 receptor agonists, heralded new possibilities in diabetes treatment when it hit the market. Originating from Gila monster saliva and sharing amino acid similarities with human GLP-1, this drug effectively reduces blood sugar levels and became a landmark addition to diabetes care by offering type 2 diabetes patients an innovative therapeutic option.
Not only does Exenatide help manage glucose control, but it also aids in weight loss for patients using the medication. The primary adverse effects associated with its use are gastrointestinal issues. These typically decrease as one’s body adjusts to the medicine and through careful dosing escalation of Exenate. Despite Bydureon—the once-weekly form of Exenate—being discontinued in 2021, many still rely on Exenate as an essential part of their regimen.
The utility of Exenate extends beyond single-drug therapy—it is approved for concurrent use with other antidiabetic agents like sulfonylureas, metformin or thiazolidinediones. This adaptability allows healthcare providers to craft customized management plans that cater specifically to each patient’s needs.
In summary, as evidence supports its effectiveness at improving glycemic measures while promoting weight reduction efforts amongst those being treated for diabetes mellitus type 2, the long-term contribution made by receptor agonist drugs such as exenetaine continues making valuable medicaments within strategies directed toward diabetic control intervention—and serves testamentally towards both progressional successes alongside forthcoming medical discoveries continually evolving within diabetological therapeutical application fields.
Trulicity: Simplifying Diabetes Management

With its once-weekly injectable regimen, Trulicity simplifies the intricate realm of diabetes management, providing a convenient substitute for daily injections for patients. This ease of use encourages better adherence to treatment plans and has been shown to significantly reduce the risk of major cardiovascular events in patients with type 2 diabetes. As a GLP-1 receptor agonist, Trulicity aids in controlling blood sugar levels, contributing to a comprehensive diabetes care approach.
The medication’s weekly dosing schedule is not only convenient, but also helps patients achieve and maintain their glycemic targets, providing sustained blood sugar control throughout the week. With the burden of daily injections lifted, individuals can focus more on other important aspects of their diabetes management, such as diet and exercise.
Trulicity’s cardiovascular benefits are particularly noteworthy, offering a reduced risk of heart-related complications for those with type 2 diabetes. This cardiovascular advantage is an essential factor to consider when selecting diabetes drugs, as it addresses one of the most common complications associated with the condition.
The role of trust in diabetes care is emblematic of the progress made in medication delivery systems, reflecting a trend towards treatments that not only improve health outcomes but also enhance the patient experience. As we continue to innovate in the field of diabetes drugs, the focus on patient-centric solutions will remain paramount.
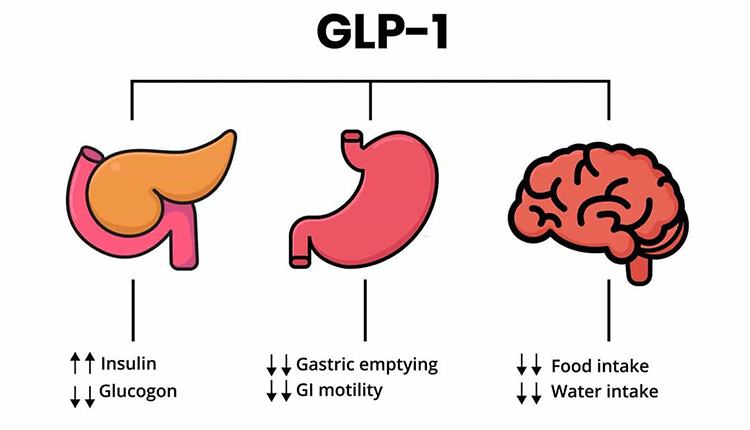
Mechanisms Behind the Magic: How GLP-1 Agonists Work
The successful action of GLP-1 agonists doesn’t happen by chance. It’s based on a clearly defined mode of operation. These medications imitate the actions of the endogenous hormone GLP-1, prompting activation of its receptor, which then sets off multiple positive metabolic responses. Among them are:
- An increase in insulin secretion
- A decrease in glucagon production
- The slowing down of gastric emptying
- An increased feeling of fullness
Such effects contribute to maintaining blood sugar levels within normal range and help curb appetite while moderating food consumption.
GLP 1 agonists exhibit their efficacy through significant improvements in both fasting and mealtime glucose readings, underpinning their pivotal status for glycemic regulation—a cornerstone in diabetes management strategies. The attribute that slows stomach emptying aids individuals to experience satiation longer after eating, thus curbing excessive food intake and supporting weight control endeavors.
Beyond targeting blood sugar stabilization, GLp 1 agonists also stand out as potent agents against obesity due to associated weight reduction benefits stemming from enhanced feelings of satiety and slowed digestive processes resulting naturally into lesser caloric intake.
Comprehending the dynamics behind how Glp 1 Agonist work provides clarity regarding their important role not only with respect to diabetes care, but also concerning obesity therapy. It is this nuanced interaction among bodily functions that enables such pharmaceuticals to furnish outcomes surpassing mere glucose level adjustments.
The Therapeutic Impact on Diabetes and Obesity
GLP-1 agonists exert a profound impact on the treatment of diabetes and obesity, providing numerous advantages that include:
- Promoting considerable weight loss
- Contributing to diminished appetite overall
- Offering potential for sustained weight management (as evidenced by 72-week studies on weight loss outcomes)
- Reducing caloric intake through suppressed hunger, which fosters better eating habits
Consequently, GLP-1 agonists stand as an important asset in endeavors towards losing and maintaining healthy body weight.
GLP1 agonists are known to enhance both cardiovascular and renal outcomes. A meta-analysis conducted in 20211 disclosed a reduction of allcause mortality by 12 percent. This is especially critical for diabetic patients who are at an increased risk of cardiac diseases. The drugs’ protective effect against kidney disease provides more value due to their influence on renal health.
The therapeutic efficacy intensifies when combining GLP1 agonists with SGLT2 inhibitors – another category of medications designed for diabetes care – offering greater control over blood sugar levels via this combined therapy approach.
Overall, the integration of GLP 1 agonists into the management strategies for diabetes and obesity marks significant progress within medical research. These therapies deliver multi-dimensional benefits toward treating these chronic illnesses thereby elevating patient quality of life while alleviating long-term health complications associated with them.
Tackling Side Effects and Contraindications
All medications have a range of possible adverse effects, and GLP-1 receptor agonists are no exception. Commonly encountered gastrointestinal side effects include nausea, vomiting, and diarrhea. These typically decrease over time with continued use of the medication. To reduce these gastrointestinal issues, patients should follow a healthy diet and stay well-hydrated. It is imperative for individuals to recognize contraindications linked with GLP-1 receptor agonists—particularly those with personal or family histories of medullary thyroid cancer or multiple endocrine neoplasia syndrome type 2—as there is an elevated risk associated with the development of malignant C-cell tumors.
When combining GLP-1 receptor agonists with other drugs that can also lower blood sugar levels, hypoglycemia becomes a significant concern. Patients must diligently check their blood glucose to prevent severe hypoglycemic episodes as well as prevent complications from diabetic retinopathy. Health professionals should be attentive in checking for indications of pancreatitis and gallbladder diseases along with symptoms suggestive of medullary thyroid carcinoma when managing patients on this class of drugs.
Comprehending the array of potential adverse reactions and contraindications related to the usage of GLP-1 agonists is critical both for practitioners administering care and patients receiving treatment so that they make informed decisions regarding safe usage while factoring in patient preferences alongside each drug’s unique profile balancing risks against benefits.
Proactive management strategies dealing precisely with side effects linked to GLIP-1 agents represent an essential pillar in leveraging their therapeutic value successfully without compromising safety measures—a process requiring constant coordination between health providers seeking optimal outcomes reflecting not only individualized medical circumstances but accommodating specific patient preferences too.
Navigating the Costs and Insurance Landscape
Affordability and insurance coverage are critical factors when it comes to GLP-1 agonists. Most Medicare and other insurance plans typically provide coverage for well-known GLP-1 agonists like Ozempic, Trulicity, and Victoza. Patients can Reduce the cost of these medications through coupons and partnerships available in the marketplace. Exenatide is another example that, while not offered as a generic yet, can be more accessible financially thanks to support from Medicare, insurance programs or pharmacy coupon discounts.
The drugs’ cost-effectiveness becomes particularly evident among individuals with cardiovascular disease. The diminished frequency of cardiovascular events due to treatment translates into significant healthcare savings over time. For people without pre-existing heart conditions, investing in these therapies still proves economically viable according to cardiovascular outcome trials—as shown by their favorable quality-adjusted life year (QALY) figures—which underscores the broader value of GLP-1 agonists in improving cardiovascular outcomes.
This extensive coverage does not extend universally across all types of GLP 1 agonists. Some options such as Wegovy and Bydureon Bcise may necessitate additional financial assistance via manufacturer’s discounts or pharmacy coupons for patients facing affordability challenges so they do not bear an excessive burden on expenses related to medical care.
The landscape navigating costs along with understanding how one’s health plan addresses medication costs involving GLP 1-agents could indeed seem daunting. Yet equipped with correct knowledge alongside various existing resources aimed at patient aid, those requiring these transformative medicines have a fair chance at acquiring them without sustaining heavy out-of-pocket expenditures thus enabling full realization of the benefits concomitant with their use.
Innovations in Drug Delivery Systems
Advancements in drug delivery systems for GLP-1 agonists are transforming the patient experience by focusing on ease-of-use and medication adherence. Oral formulations are particularly promising, offering an attractive alternative to injectable options. Oral semaglutide, for example, circumvents the challenges of enzyme degradation and intestinal permeability by incorporating a carrier molecule to enhance absorption.
The transition to oral medication is not without its challenges, but the potential for increased patient adherence makes it a worthwhile pursuit. The use of carriers like sodium N-(8-[2-hydroxybenzoyl] amino) caprylate (SNAC) in oral serum is a testament to the ingenuity being applied to overcome these obstacles.
Weekly injection regimens, such as those adopted by some GLP-1 receptor agonists, have already been met with patient preference due to the reduced frequency of administration compared to daily injections like basal insulin. These advancements reflect a deeper understanding of patient needs and a commitment to improving the overall management of chronic conditions like diabetes and obesity.
As we continue to push the boundaries of what’s possible, the collaboration between researchers, healthcare providers, and compounding pharmacies will be crucial in developing and refining drug delivery systems that meet the demands of modern medical care. The future of diabetes drugs is one where efficacy is matched with patient-centric solutions, ensuring that treatments are not only effective but also seamlessly integrated into daily life.
Beyond Blood Sugar: Additional Health Benefits
GLP-1 receptor agonists have benefits that extend far beyond the management of blood sugar. These receptor agonists are recognized for their cardioprotective properties and have been approved by the FDA to lower the risk of major adverse cardiovascular events in individuals who are overweight or obese with cardiovascular disease. This is particularly significant for those with diabetes, as they face an elevated risk for heart conditions.
GLP-1 receptor agonists are linked to enhancements in kidney function. There have also been instances where patients experienced acute kidney injury and renal insufficiency while on these medications. Consequently, it’s vital that patients collaborate closely with healthcare professionals to track renal function carefully during treatment.
There’s growing evidence suggesting a positive role of GLP-1 agonists in managing polycystic ovary syndrome (PCOS) and non-alcoholic fatty liver disease (NAFLD), providing new avenues for addressing these difficult-to-treat disorders. The potential anti-depressant and neuroprotective actions broaden their therapeutic scope.
The influence of GLP-1 agonors reflects a comprehensive perspective on health care within diabetes management—emphasizing more than just blood sugar control but contributing to wider health outcomes through various other additional patient well-being aspects.
The Role of Lifestyle Changes in GLP-1 Agonist Therapy
When combined with a balanced diet and consistent exercise, the efficacy of GLP-1 agonist treatment is significantly enhanced. There’s a mutually strengthening relationship between these medications and lifestyle changes. Each element is essential for reaching glycemic goals and managing weight-related complications. Patients who adopt nutritious eating habits and elevate their physical activity levels can intensify the benefits of weight loss and health improvements brought on by medicines such as Semaglutide, among other GLP-1 agonists.
To maintain progress achieved through GLP-1 agonist therapy, continuous dedication to lifestyle interventions is necessary rather than just an initial attempt at improvement. To avoid regaining weight after stopping medication use, long-term maintenance of healthy lifestyles is critical. Healthcare professionals usually recommend harmonizing GLP-1 agonists with alterations in way of life to enhance outcomes in treating type 2 diabetes care—a strategy that typically involves:
- Engaging in regular workouts
- Adopting nutritional dietary patterns
A commitment to keeping track of bodyweight management.
Employing methods to mitigate stress.
And quit smoking.
These behavioral shifts not only boost the potency but also improve overall wellness when integrated into one’s regimen alongside taking GLD 7:17 pm PSTest drugs.
Incorporating this comprehensive method highlights patient education’s role along with support within diabetes care enabling individuals’ greater control over their treatments via well-informed adjustments behaviorally optimizes therapeutic actions using glucose-like peptide (GLG) receptor ligands leads to better results terms headway made against illnesses – indeed it does represent momentous opportunity for betterment ones situation pertaining ailments aforementioned types.
It remains integral towards crafting tailored healthcare plans including both pharmacological solutions involving agents acting upon receptors related peptides possessing similarities glucagon line addition various adaptive behaviors considering entirety complexities accompanying disorder thus ushering era where afflicted parties may find solace comfort ability effectively tackle obstacles arise due predicaments stemming from diabetic syndromes more manageable align themselves trajectory points optimism personal growth possibility genuine happiness newfound sense fulfillment likely ensue thereafter ensuing interactions collaborations set forth before them accordingly therein lies potential transformative experiences await those willing engage actively participate journey ahead full realization potentials lie beyond horizon yet reached embraced its fullest extent possible given present circumstances constraints thereof mindfully aware implications therein associated therewith henceforth moving forward collective future bright hopeful promise beckons call action answer willingly courageously nobly venture chart course destiny designed excellence perpetuity amen
Summary
As we conclude our journey through the world of GLP-1 agonists, it’s clear that these medications are a powerful force in the battle against diabetes and obesity. They offer a multifaceted approach to treatment, providing blood sugar control, weight management, and a suite of additional health benefits that extend well beyond glycemic efficacy. The innovations in drug delivery systems and the importance of combining pharmacotherapy with lifestyle changes underscore the dynamic and evolving nature of diabetes care.
Ultimately, the goal is to empower patients to lead healthier, more fulfilling lives by providing them with the tools and knowledge they need to manage their condition effectively. GLP-1 agonists are a testament to the progress made in medical science and the commitment to finding solutions that cater to the needs of individuals living with chronic diseases. May this guide serve as a beacon, illuminating the path to better health and inspiring those affected by diabetes and obesity to take control of their treatment journey.
Frequently Asked Questions
Meet the Author

Bradley Keys
Bradley Keys is an accomplished writer who has covered a wide variety of health, nutrition, and wellness topics. He graduated with a Bachelor of Science from Florida State University, and has extensively explored a diverse range of subjects within the realms of health, wellness, and nutritional supplementation, showcasing a broad and in-depth understanding of these interconnected fields.
Reviewed by :

Dr. Majid Sabour
Dr. Majid Sabour, MD, is a renowned expert in medical weight loss and the founder and medical director of Gent's Doctor clinic in Beverly Hills, California. With over 25 years of experience, Dr. Sabour is board-certified in family medicine and specializes in helping patients achieve their weight loss goals through personalized medical treatments. He graduated from Zaporizhzhia State Medical University in Ukraine and completed a family medicine residency program with Columbia University and Cornell at New York-Presbyterian Hospital in Manhattan. Licensed in both New York and California, Dr. Sabour is dedicated to providing comprehensive weight loss solutions that promote overall health and well-being.